Sinusitis
in brief.
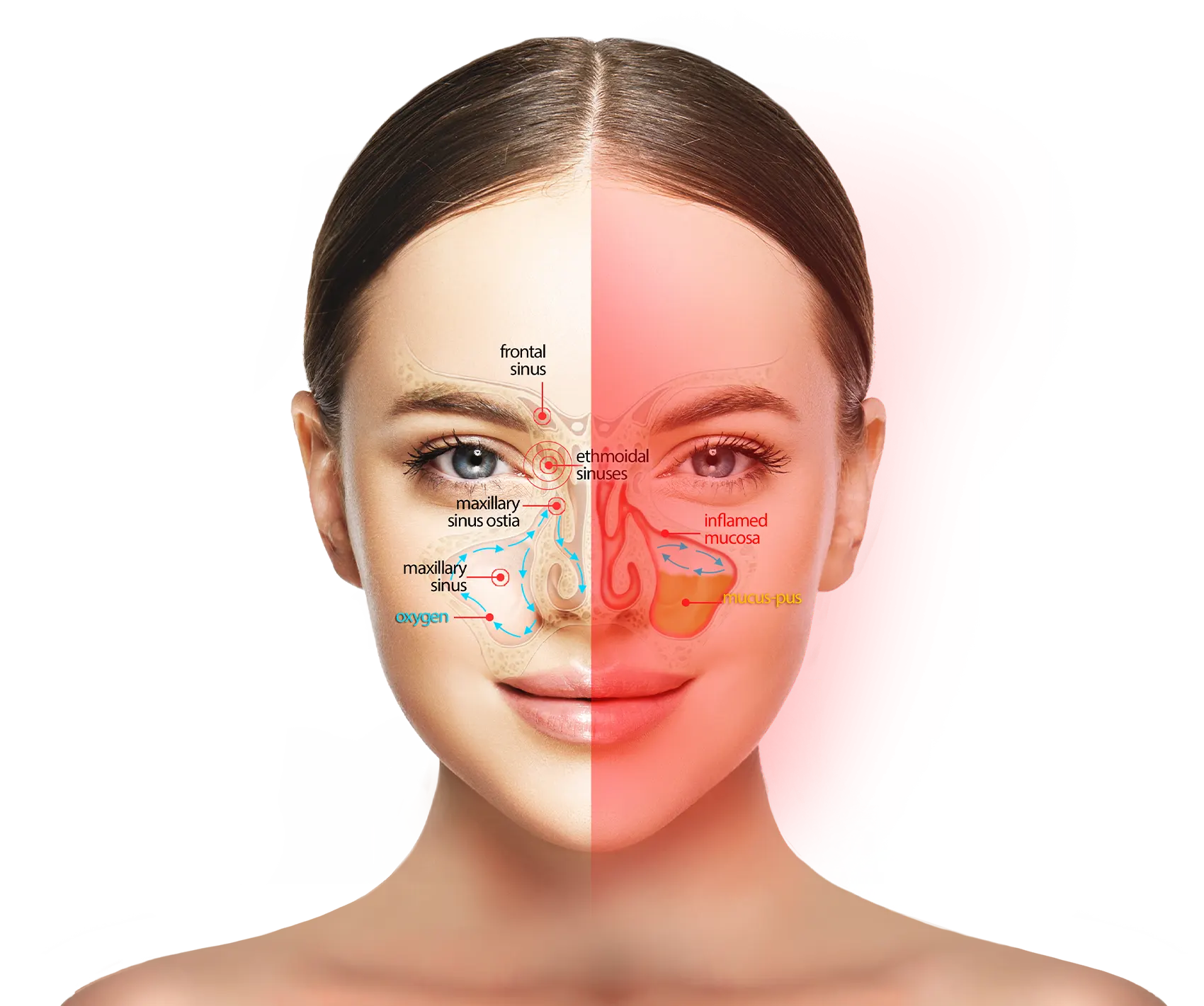
Rhinosinusitis is an inflammation of the respiratory mucosa affecting the nose, nasal cavities, and sinus ostia, whether or not accompanied by an infectious process.
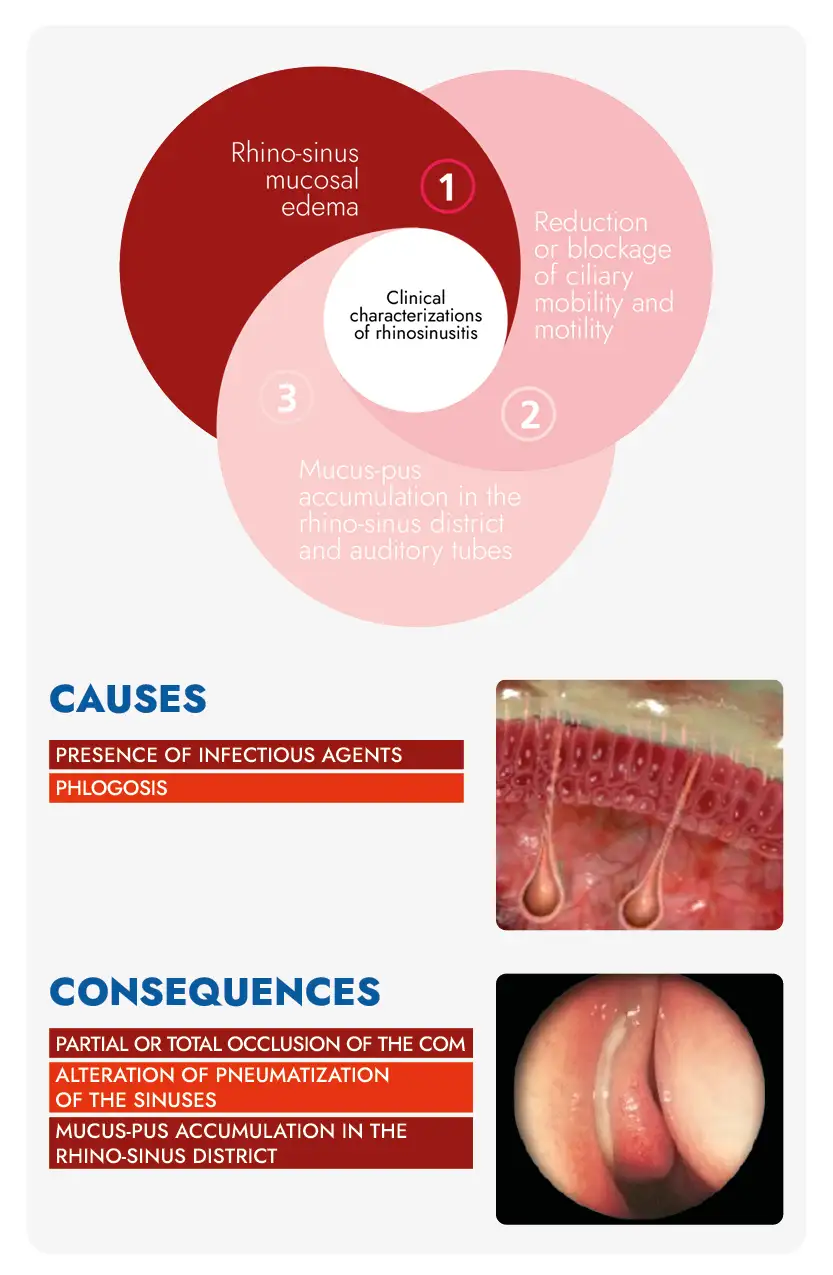
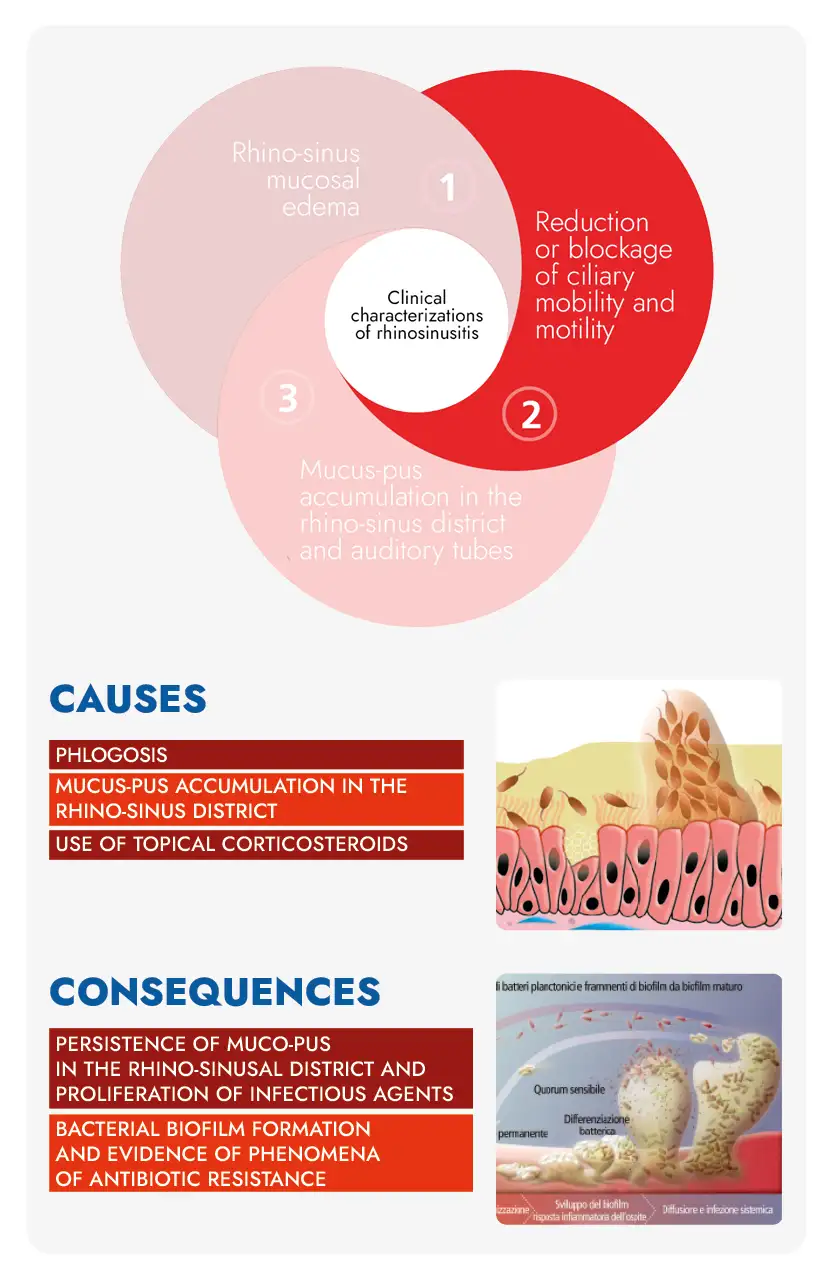
The most important clinical characterizations of rhinosinusitis are:
- Edema of the rhino-sinus mucosa
- Reduction or blockage of ciliary mobility and motility
- Accumulation of muco-purulent secretions in the rhinosinusal districte and in the auditory tubes
CLINICAL CHARACTERIZATIONS
OF RHINOSINUSITIS
What are the symptoms of rhinosinusitis?
The symptoms of rhinosinusitis can vary depending on the etiology, that is, the factor or factors that caused it.
Rhinosinusitis
infectious.
Symptoms
- Mucus discharge from the nose that is yellow or greenish in color, or you find it on the handkerchief when you blow your nose
- Facial pain in one or more places (above the jaws, around the eyes at the sides of the nose, at the forehead above the eyebrow arches, in the back of the skull)
- Sensation of not being able to smell
- Nosebleed
- Mucus going down the throat
- Symptoms in only one nostril of the nose (nasal obstruction, presence of purulent mucus, bleeding)
Causes
A very commonplace cold that lasts for more than 5-7 days, brought on by an infection caused by viruses, fungi, and/or pathogenic bacteria (Infectious rhinosinusitis)
Rhinosinusitis
allergic.
Symptoms
- Mucus discharge from the nose almost as clear as water, indistinctly from both nostrils
- Frequent sneezing even without the discharge of mucus from the nose
- Itchy nose
- Facial pain in one or more places (above the jaws, around the eyes at the sides of the nose, at the forehead above the eyebrow arches, in the back of the skull)
- Conjunctivitis with red or itchy eyes
Causes
An underlying respiratory allergy, caused by exposure to particular types of allergens such as pollens, dust mites, chemicals…
Rhinosinusitis
non-allergic
cell-mediated.
Symptoms
- Mucus discharge from the nose almost as clear as water, indistinctly from both nostrils
- Frequent sneezing even without the discharge of mucus from the nose
- Itchy nose
- Facial pain in one or more places (above the jaws, around the eyes at the sides of the nose, at the forehead above the eyebrow arches, in the back of the skull)
- Conjunctivitis with red or itchy eyes
Causes
The presence of non-allergic cell-mediated rhinitis, caused by the dysfunction of certain cells found in the respiratory mucosa such as: mast cells, eosinophils and neutrophils). Depending on the cells affected by the dysfunction, the following cellular diseases are distinguished: nares , narne, narma, and naresma – nonallergic cell-mediated rhinosinusitis
The following may also be present in all cases: photophobia, difficulty concentrating, and general malaise.
In infectious rhinosinusitis, the same symptoms may be accompanied by fever.
Regarding pain in rhinosinusitis, there is a myth to dispel, namely that pain results from inflammation of the respiratory mucosa. Actually, the pain that is felt is craniofacial pain, that is, neuropathic pain: in other words, pain resulting from inflammation (stimulation) of craniofacial nerves.
Basically what happens?
It is as simple as that! When the inflammation extends beyond the nasal cavities (about 5-7 days after what we can classify as a common cold), the same inflammation is also beginning to affect the mucosa lining the ostia of the paranasal sinuses (small 1-2 mm diameter ducts that connect the nasal passages to the paranasal sinuses). When it becomes inflamed, the mucosa increases in volume: because the ostia are very narrow, it results in the narrowing of their internal lumen until they become occluded. When the ostium of a paranasal sinus is occluded, two very important functions of the latter are altered, namely: stopping the flow of mucus from the paranasal sinuses to the sinus cavities of the nose (thus outward) and, most importantly, preventing the transit of oxygen from the nose to the paranasal sinuses. Stopping the transit of oxygen in the sinuses, in fact, results in the onset of neuropathic pain, or inflammation of the craniofacial nerves.
When an ostium is occluded, the paranasal sinus connected to it takes on the appearance of an air-filled balloon closed at the end. The walls of the paranasal sinus are not impermeable to air as they are lined with ciliated mucosa in which blood vessels are present: these vessels will more or less quickly absorb oxygen trapped in the sinus.
When this has been totally depleted, a depression will be created within the sinus that produces a physical force that tends to attract the mucous membrane toward the center of the paranasal sinus, as if the latter wanted to detach itself from the bone to which it is anchored. Just what happens when we force air out of a balloon and its walls tend to stick to each other.
Rhinosinusitis: pain and infection
Obviously, the mucosa does not only consist of hair cells, mucipar cells, blood vessels etc. but also of nerve fibers connected to craniofacial nerves. Therefore, when there is the establishment of depression i.e., negative pressure from the outside to the inside, there is a mechanical stress on the nerve fibers that is transmitted and reflected on the craniofacial nerves and from which pain originates.
Moreover, if the situation of complete obstruction of the ostium remains unchanged, as soon as the trapped oxygen is completely depleted, a new process intended to increase pain: the mucosa lining the sinuses will begin to produce a large amount of mucus that evidently cannot exit the affected sinus due to obstruction of the ostium. The mucus itself, then, will eventually exert positive pressure against the mucosa lining the breast (i.e., outward), putting more stress on the nerve fibers and accentuating the pain.
Although what has been highlighted so far summarizes a disastrous situation at the clinical level, the trouble is not over yet: should the situation of the obstruction of the ostium continue much longer, the mucus that has accumulated in the affected sinus, will become infected due to certain pathogenic bacteria that manage in various ways to enter the same sinus. The pain will be overlaid with infection and thus the need to take large amounts of antibiotics.
First, there is a distinction to be made based on the type of rhinosinusitis:
- Infectious rhinosinusitis becomes chronic when infected mucus accumulates within one or more sinuses for a long time that fails to be evacuated, and from this inflammation arises that continues over time
- Allergic rhinosinusitis becomes chronic when we remain exposed to an allergenic substance or agent for a long time and is not treated with appropriate medication
- Non-allergic cell-mediated rhinosinusitis (NARES, NARNE, NARMA AND NARESMA) becomes chronic when this is not diagnosed and treated in a timely manner with appropriate and specific drugs (at present there are no highly specific pharmaceuticals for this condition)
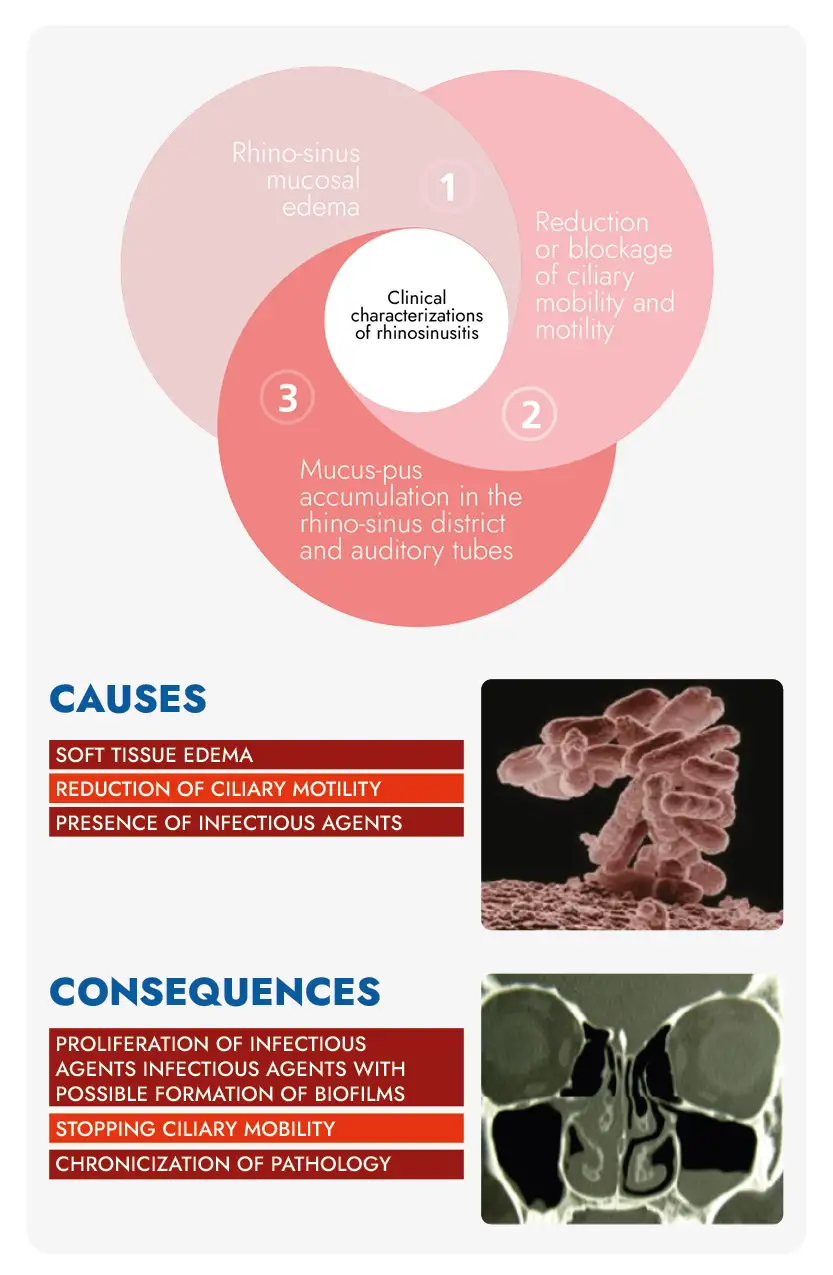
In any case, whatever the type of rhinosinusitis, the factors that lead to chronicity of the condition can be summarized as follows:
- Edema (enlargement) of the rhino-sinus mucosa resulting from protracted inflammation
- Slowdown or even arrest of ciliary cell mobility and motility
What are hair cell cilia?
The respiratory mucosa is nothing more than a lining of the entire respiratory system, thus of the nasal passages, ostia, and sinuses (this as far as the upper respiratory tract is concerned). The mucosa consists on the outer surface of essentially two types of cells: ciliated cells and mucipar cells. Hair cells are equipped with cilia i.e., small appendages whose main task is to move mucus outward, like real brushes. If for any reason the cilia do not or cannot move, the mucus remains stationary in the various cavities of the respiratory system. When mucus is unable to be evacuated to the outside and remains stationary in the cavities of the respiratory system, it sooner or later becomes infected and produces inflammation.
What is meant by ciliary mobility?
Ciliary mobility represents the ability of cilia of hair cells to move. The main impediment to their movement is the presence of a very thick and fatty mucus blanket that literally traps them and prevents their movement. This occurs when mucus stagnates for a long time in the upper respiratory cavity because it is not expelled in a timely manner.
What is meant by ciliary motility?
Ciliary motility represents the frequency of ciliary movement that is, the speed of cilia movement. Normally, the cilia of the hair cells move to transport mucus outward with a definite frequency (ciliary beat): this frequency is drastically reduced when mucous membrane inflammation and stagnation of mucus-pus in the upper respiratory cavities persist for a long time.
What to do in case of rhinosinusitis?
Treating rhinosinusitis is by no means a simple matter for two essential reasons:
- it is necessary to make a precise diagnosis of the etiology of rhinosinusitis i.e. to determine exactly the factor or factors that caused it
- depending on the diagnosed etiology and the stage of the pathology, determine the most appropriate therapy to be practiced
Of course, in order to have an accurate diagnosis, it is necessary to consult an ENT specialist and if necessary, consult the allergist, pulmonologist, and possibly the cytologist.
In the case of rhinosinusitis in children, it is advisable to consult the pediatrician first and then possibly the medical specialists mentioned above, provided that the latter are familiar with children, given their fragile relationship with the physician in general. Nevertheless, today it is possible to perform a test to get an indication of the possible diagnosis of rhinosinusitis through the development of a diagnostic algorithm developed by our researchers.
Rhinosinusitis? Make the Diagnosis online.
-
 Get diagnostic outcomes in minutes
Get diagnostic outcomes in minutes Diagnostic outcomes in minutes
Diagnostic outcomes in minutes Discover the treatment that’s right for you
Discover the treatment that’s right for you Discover the right drugs
Discover the right drugs Simple to use, and reliable
Simple to use, and reliable 100% Effectiveness
100% Effectiveness
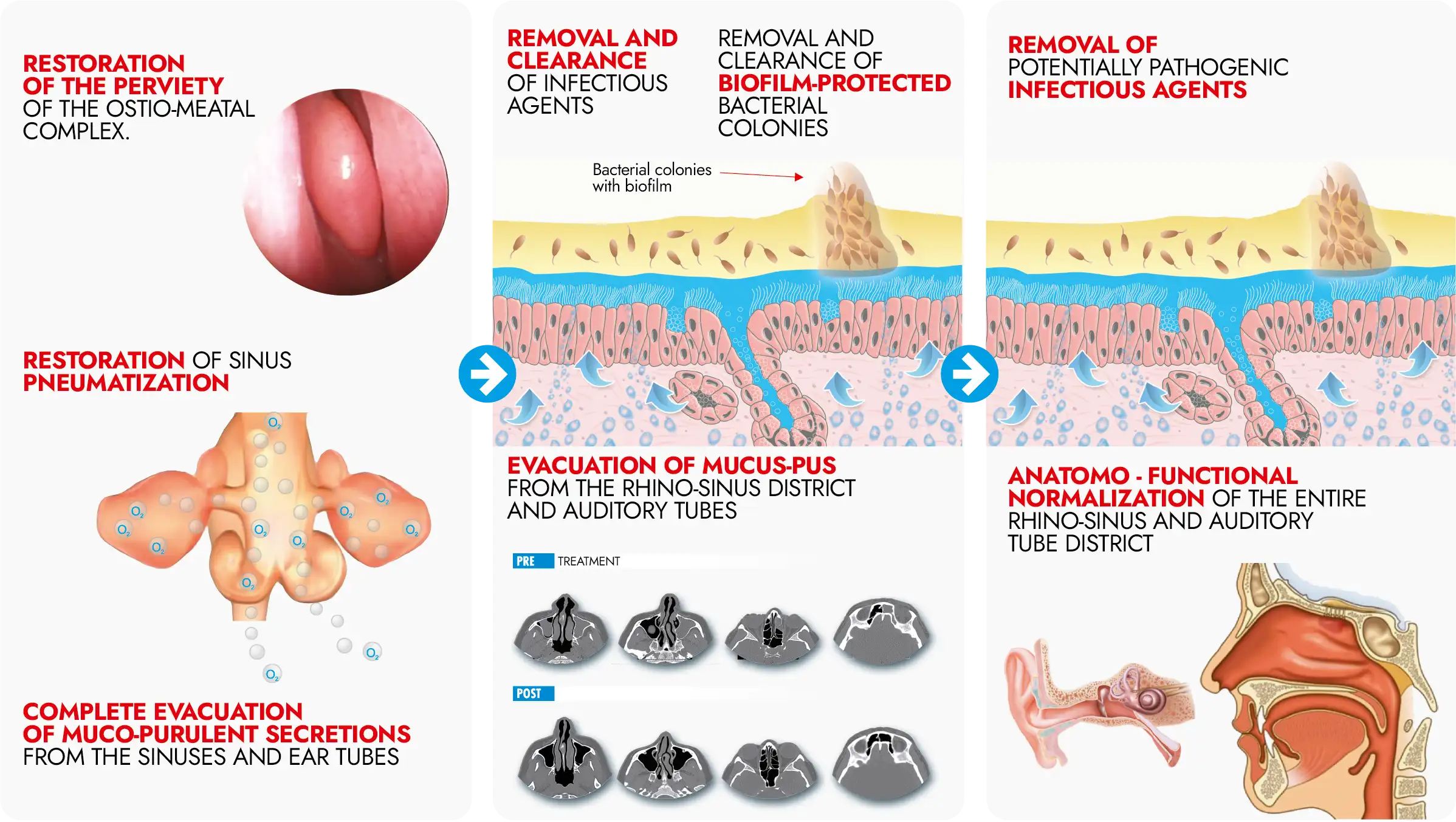
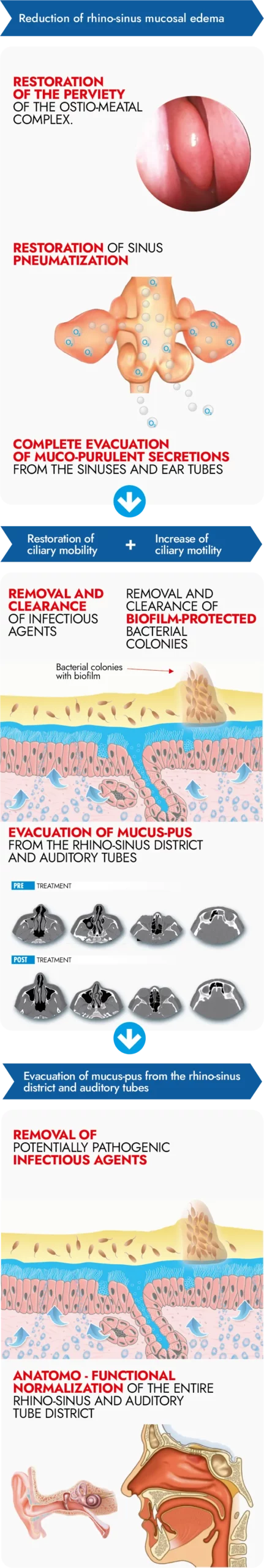
The therapeutic goals to treat
effectively rhinosinusitis

Characteristics and benefits of the most widely used pharmaceutical products
Below is a table summarizing the characteristics and benefits of the pharmaceutical products most widely used to date to treat rhinosinusitis, in relation to the three clinical characterizations of the same condition.
Scroll down the table
| Product category | Reduction of mucosal edema | Evacuation of mucus from the rhino-sinus district | Restoration or stimulation of ciliary mobility and motility | Notes |
|---|---|---|---|---|
| Antibiotics | No | No | No | They act only on pathogenic bacteria, not on viruses and fungi. They cannot penetrate inside the sinuses, so they are not effective in eradicating the infection in the mucus. |
| Corticosteroids | Yes, in an indirect way | No | No, vice versa they depress it | Corticosteroids, act only on inflammation by reducing it, but not on mucosal edema (swelling). Reduction of edema occurs physiologically after several days of treatment. At the same time, they exert no action on the fluidization and defluxation of mucus. They slow down ciliary motility, the only system for mucus to flow outward. |
| Mucolytics | No | Yes, only from the nasal passages, no from the ostia and sinuses | Yes, only of ciliary motility and only in the nasal pits, no action on ciliary motility | Fluidizing mucus, does not always mean evacuating it, as, by not acting on the edema, the osti remain closed. In addition, mucolytics cannot penetrate the sinuses. |
| Decongestants | Yes, only for a few hours | No | No | They result in the reduction of mucosal edema quickly and the quick disappearance of pain, but only for a short time (hours). They are addictive and often produce the opposite of the desired effect if used for a long time. |
| Hypertonic Saline Solution | Yes, only in the nasal passages, not in the sinuses and ostia | Yes, only in the nasal passages, not in the sinuses and ostia | Yes, only of ciliary motility and only in the nasal pits, no action on ciliary motility | It is certainly a very effective medium in the nasal passages, that is, as far as it can exert its action. Obviously not at all effective in rhinosinusitis, which evidently also affects the ostia and sinuses. |
| Isotonic Salt Solution | No | No | No | They are very useful in prevention for at-risk individuals; used frequently in the absence of pathology, they help keep the mucosa clean and efficient. |
| Cucurbitacins B-D-I-E (CiliaCell) |
Yes | Yes | Yes | Cucurbitacins B-D-I-E (CiliaCell) act simultaneously on the 3 clinical characterizations of Rhinosinusitis by effectively restoring the anatomic-functional conditions of the upper respiratory tract and promote the rapid disappearance of symptoms. Cucurbitacins B-D-I-E act on the entire respiratory epithelium, therefore; on both the nasal mucosa and the ostia and sinuses, despite being administered into the nostrils with a simple nasal spray. |


THERAPEUTIC ACTIONS
CUCURBITACINS B-D-I-E
See the effectiveness of treatment with CiliaCell
On the three clinical characterizations of rhinosinusitis
1- REDUCTION OF EDEMA
2 – RESTORATION OF MOBILITY AND CILIAR MOBILITY.
3 – EVACUATION OF MUCUS-PUS
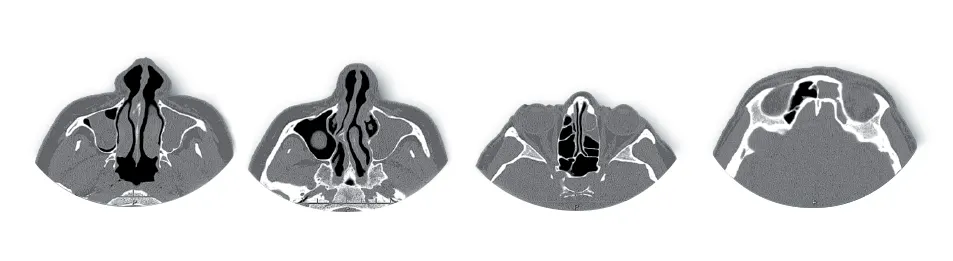 Before Treatment with CiliaCell
Before Treatment with CiliaCell After Treatment with CiliaCell
After Treatment with CiliaCellView the efficacy
of
treatment with CiliaCell
on the three
clinical characterizations of rhinosinusitis
1- REDUCTION OF EDEMA
2 – RESTORATION OF MOBILITY AND CILIAR MOBILITY.
3 – EVACUATION OF MUCUS-PUS
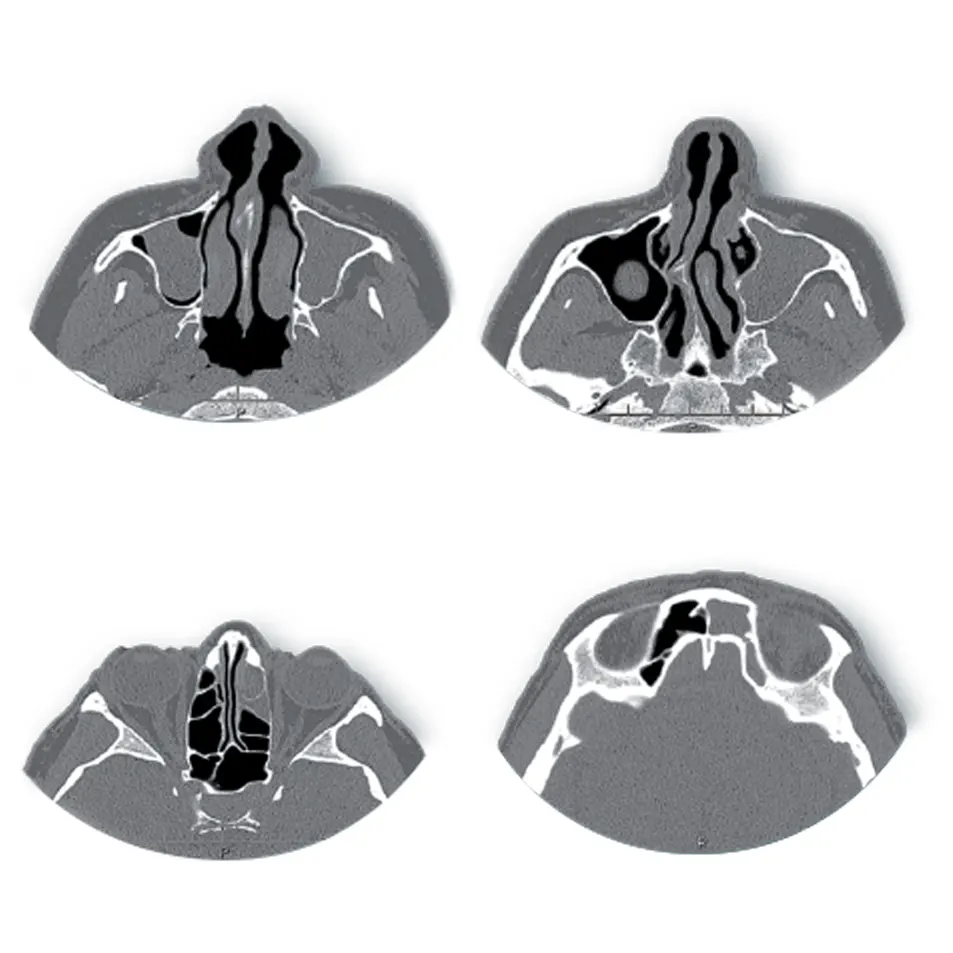 Prima del Trattamento con CiliaCell
Prima del Trattamento con CiliaCell Dopo il Trattamento con CiliaCell
Dopo il Trattamento con CiliaCellDepending on the etiology of rhinosinusitis, a specific product would be needed that acts not only on the symptom, but also on the cause of the pathology, otherwise there is a risk of only achieving more or less effective symptom resolution, but not effectively treating the cause of the same pathology.
Today there are many pharmaceuticals on the market used to treat rhinosinusitis that almost always act only on the symptoms, except for antibiotics that act on the pathogens responsible for the disease if present. Obviously, these act only on pathogenic bacteria, so they are not at all effective against viral infections (which account for 85% of the etiological agents of rhinosinusitis) and fungal infections. In this regard, it is estimated that only 5% of infectious rhinosinusitis is bacterial in origin. Nevertheless, there is a need to point out that bacterial infection almost always overlaps with viral infection, especially if the latter is not promptly eradicated.
A product specifically indicated in the treatment of rhinosinusitis, whatever the etiology (cause), should act simultaneously on the three clinical characterizations of rhinosinusitis, viz:
- Edema of the rhino-sinus mucosa due to inflammation
- the slowing or even stopping of ciliary mobility and motility (the only means by which mucus can be evacuated from the entire rhino-sinus district i.e., from the nose to the paranasal sinuses. Mucus cannot drain without the action of the cilia of the ciliated cells)
- The accumulation of muco-purulent secretions in the rhino-sinus region and auditory tubes, if present
Today, there is a product on the market specifically for rhinosinusitis characterized by precisely all three of the above clinical manifestations.